Medical Precertification Request Form Humana . Use the links below to submit the preauthorization form, find other forms or learn more about the. humana manages the pharmacy drug benefit for your patient. Decision & notification are made within 14 calendar days* for hmsa. standard request for medicare and medicaid plans: humana manages the pharmacy drug benefit for your patient. medical precertification request form eoc id: Search by current procedural terminology (cpt). find frequently requested services and procedures below to submit prior authorizations for your humana medicare or commercial patients. Certain requests for precertification may require additional. your doctor or healthcare provider can submit inpatient and outpatient referral, prior authorization and. easily determine if a prior authorization is required with our search tool. Certain requests for precertification may.
from www.pdffiller.com
medical precertification request form eoc id: Certain requests for precertification may. find frequently requested services and procedures below to submit prior authorizations for your humana medicare or commercial patients. Decision & notification are made within 14 calendar days* for hmsa. humana manages the pharmacy drug benefit for your patient. humana manages the pharmacy drug benefit for your patient. easily determine if a prior authorization is required with our search tool. Use the links below to submit the preauthorization form, find other forms or learn more about the. standard request for medicare and medicaid plans: Certain requests for precertification may require additional.
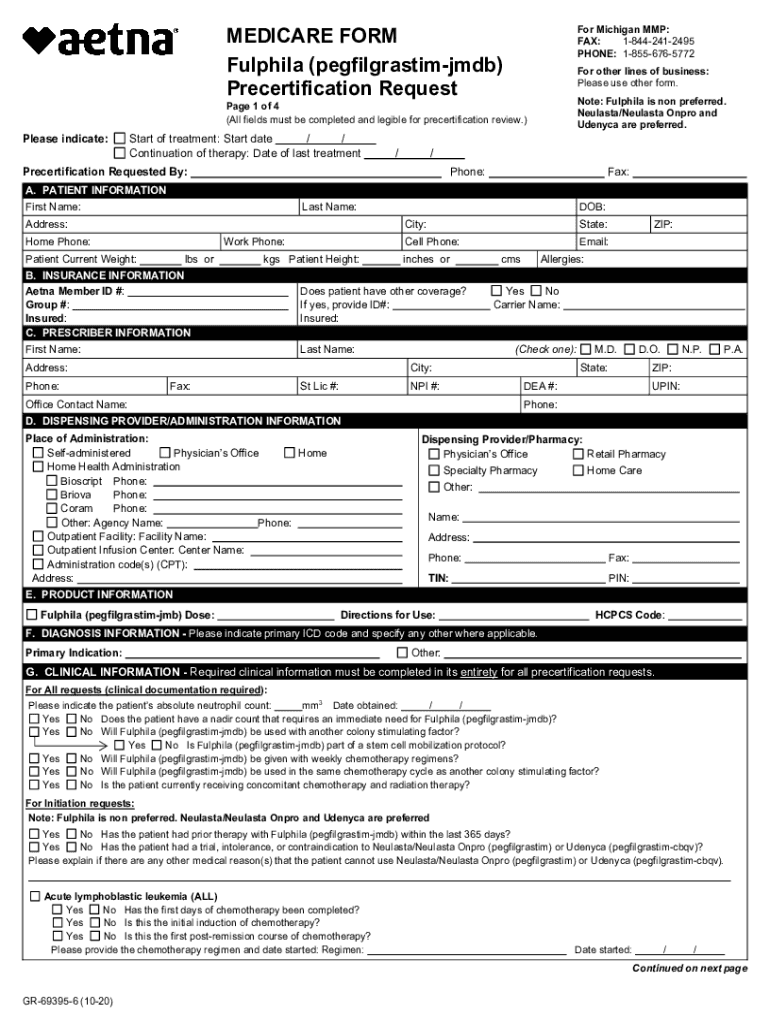
Fillable Online MEDICARE FORM Precertification Request Fax Email Print
Medical Precertification Request Form Humana Use the links below to submit the preauthorization form, find other forms or learn more about the. Search by current procedural terminology (cpt). humana manages the pharmacy drug benefit for your patient. Use the links below to submit the preauthorization form, find other forms or learn more about the. easily determine if a prior authorization is required with our search tool. your doctor or healthcare provider can submit inpatient and outpatient referral, prior authorization and. standard request for medicare and medicaid plans: humana manages the pharmacy drug benefit for your patient. find frequently requested services and procedures below to submit prior authorizations for your humana medicare or commercial patients. Decision & notification are made within 14 calendar days* for hmsa. medical precertification request form eoc id: Certain requests for precertification may. Certain requests for precertification may require additional.
From www.pdffiller.com
20222024 Humana Medical Precertification Request Form Fill Online Medical Precertification Request Form Humana humana manages the pharmacy drug benefit for your patient. humana manages the pharmacy drug benefit for your patient. medical precertification request form eoc id: Certain requests for precertification may require additional. Decision & notification are made within 14 calendar days* for hmsa. Search by current procedural terminology (cpt). standard request for medicare and medicaid plans: Certain. Medical Precertification Request Form Humana.
From www.vrogue.co
Printable Humana Radiology Precertification Request F vrogue.co Medical Precertification Request Form Humana medical precertification request form eoc id: Certain requests for precertification may require additional. your doctor or healthcare provider can submit inpatient and outpatient referral, prior authorization and. standard request for medicare and medicaid plans: Certain requests for precertification may. easily determine if a prior authorization is required with our search tool. Use the links below to. Medical Precertification Request Form Humana.
From www.pdffiller.com
United Healthcare Prior Authorization Forms Fill Online, Printable Medical Precertification Request Form Humana Use the links below to submit the preauthorization form, find other forms or learn more about the. Certain requests for precertification may. standard request for medicare and medicaid plans: humana manages the pharmacy drug benefit for your patient. your doctor or healthcare provider can submit inpatient and outpatient referral, prior authorization and. easily determine if a. Medical Precertification Request Form Humana.
From www.formsbank.com
Fillable Humana Universal Fax Form For Drug Authorization printable pdf Medical Precertification Request Form Humana your doctor or healthcare provider can submit inpatient and outpatient referral, prior authorization and. Decision & notification are made within 14 calendar days* for hmsa. Certain requests for precertification may. medical precertification request form eoc id: Certain requests for precertification may require additional. humana manages the pharmacy drug benefit for your patient. Use the links below to. Medical Precertification Request Form Humana.
From www.uslegalforms.com
United Healthcare Referral Form Pdf 2020 Fill and Sign Printable Medical Precertification Request Form Humana medical precertification request form eoc id: Use the links below to submit the preauthorization form, find other forms or learn more about the. Certain requests for precertification may. find frequently requested services and procedures below to submit prior authorizations for your humana medicare or commercial patients. Certain requests for precertification may require additional. standard request for medicare. Medical Precertification Request Form Humana.
From www.reviewhome.co
Humana Home Health Authorization Request Form Review Home Co Medical Precertification Request Form Humana Certain requests for precertification may. standard request for medicare and medicaid plans: medical precertification request form eoc id: humana manages the pharmacy drug benefit for your patient. Certain requests for precertification may require additional. find frequently requested services and procedures below to submit prior authorizations for your humana medicare or commercial patients. Search by current procedural. Medical Precertification Request Form Humana.
From www.sampleforms.com
FREE 13+ Prior Authorization Forms in PDF MS Word Medical Precertification Request Form Humana Decision & notification are made within 14 calendar days* for hmsa. Use the links below to submit the preauthorization form, find other forms or learn more about the. Certain requests for precertification may. Certain requests for precertification may require additional. easily determine if a prior authorization is required with our search tool. your doctor or healthcare provider can. Medical Precertification Request Form Humana.
From fill.io
Fill Free fillable Aetna Health Insurance PDF forms Medical Precertification Request Form Humana Certain requests for precertification may. humana manages the pharmacy drug benefit for your patient. Search by current procedural terminology (cpt). easily determine if a prior authorization is required with our search tool. medical precertification request form eoc id: Decision & notification are made within 14 calendar days* for hmsa. your doctor or healthcare provider can submit. Medical Precertification Request Form Humana.
From www.youtube.com
All About Precertification YouTube Medical Precertification Request Form Humana easily determine if a prior authorization is required with our search tool. your doctor or healthcare provider can submit inpatient and outpatient referral, prior authorization and. find frequently requested services and procedures below to submit prior authorizations for your humana medicare or commercial patients. Certain requests for precertification may require additional. Use the links below to submit. Medical Precertification Request Form Humana.
From www.vrogue.co
Humana Medical Precertification Request Form Fill And vrogue.co Medical Precertification Request Form Humana your doctor or healthcare provider can submit inpatient and outpatient referral, prior authorization and. humana manages the pharmacy drug benefit for your patient. Search by current procedural terminology (cpt). Certain requests for precertification may. medical precertification request form eoc id: Certain requests for precertification may require additional. standard request for medicare and medicaid plans: Decision &. Medical Precertification Request Form Humana.
From www.formsbank.com
Fillable Form Gr68774 Medication Precertification Request Form Medical Precertification Request Form Humana medical precertification request form eoc id: find frequently requested services and procedures below to submit prior authorizations for your humana medicare or commercial patients. easily determine if a prior authorization is required with our search tool. Certain requests for precertification may require additional. Use the links below to submit the preauthorization form, find other forms or learn. Medical Precertification Request Form Humana.
From eforms.com
Free Humana Prior (Rx) Authorization Form PDF eForms Medical Precertification Request Form Humana Search by current procedural terminology (cpt). standard request for medicare and medicaid plans: your doctor or healthcare provider can submit inpatient and outpatient referral, prior authorization and. humana manages the pharmacy drug benefit for your patient. Certain requests for precertification may require additional. Use the links below to submit the preauthorization form, find other forms or learn. Medical Precertification Request Form Humana.
From www.vrogue.co
Printable Humana Radiology Precertification Request F vrogue.co Medical Precertification Request Form Humana medical precertification request form eoc id: Decision & notification are made within 14 calendar days* for hmsa. Use the links below to submit the preauthorization form, find other forms or learn more about the. Certain requests for precertification may require additional. easily determine if a prior authorization is required with our search tool. humana manages the pharmacy. Medical Precertification Request Form Humana.
From www.vrogue.co
Humana Medical Precertification Request Form Fill And vrogue.co Medical Precertification Request Form Humana find frequently requested services and procedures below to submit prior authorizations for your humana medicare or commercial patients. Use the links below to submit the preauthorization form, find other forms or learn more about the. Certain requests for precertification may require additional. Search by current procedural terminology (cpt). easily determine if a prior authorization is required with our. Medical Precertification Request Form Humana.
From www.vrogue.co
Printable Humana Radiology Precertification Request F vrogue.co Medical Precertification Request Form Humana Decision & notification are made within 14 calendar days* for hmsa. your doctor or healthcare provider can submit inpatient and outpatient referral, prior authorization and. find frequently requested services and procedures below to submit prior authorizations for your humana medicare or commercial patients. Use the links below to submit the preauthorization form, find other forms or learn more. Medical Precertification Request Form Humana.
From www.uslegalforms.com
Humana Prior Authorization Request Form Fill and Sign Printable Medical Precertification Request Form Humana easily determine if a prior authorization is required with our search tool. Search by current procedural terminology (cpt). humana manages the pharmacy drug benefit for your patient. Decision & notification are made within 14 calendar days* for hmsa. find frequently requested services and procedures below to submit prior authorizations for your humana medicare or commercial patients. Use. Medical Precertification Request Form Humana.
From www.formsbank.com
Form 5203 Humana Critical Illness Claim Form G&g Associates Medical Precertification Request Form Humana find frequently requested services and procedures below to submit prior authorizations for your humana medicare or commercial patients. humana manages the pharmacy drug benefit for your patient. humana manages the pharmacy drug benefit for your patient. Decision & notification are made within 14 calendar days* for hmsa. Search by current procedural terminology (cpt). Use the links below. Medical Precertification Request Form Humana.
From www.formsbank.com
Referral Prior Authorization Form Kern Legacy Health Plan printable Medical Precertification Request Form Humana find frequently requested services and procedures below to submit prior authorizations for your humana medicare or commercial patients. easily determine if a prior authorization is required with our search tool. Certain requests for precertification may require additional. humana manages the pharmacy drug benefit for your patient. humana manages the pharmacy drug benefit for your patient. Use. Medical Precertification Request Form Humana.